- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2025
Travel History & Diagnostic Decision Support Tools in the Ebola Fight
I wrote about Ebola and the importance of mobile diagnosis decision support in 2012 when the last outbreak occurred. Now in 2014, West Africa is experiencing the worst outbreak of Ebola in history with as many as 7000 people diagnosed and 3,338 people who have died from the disease. However, these figures may be underestimated due to under reporting and the fact that many cases are not counted as people aren’t attending health care facilities due to lack of transport or as they are full and closed to new admissions.
In the USA, media articles are reporting the Dallas Ebola case of Eric Duncan who had helped carry a pregnant woman in Liberia who was desperately ill with Ebola. Mr Duncan then returned to the USA and presented twice at a hospital with Ebola symptoms, unfortunately he was not diagnosed until his second visit when he presented with severe symptoms. During his first visit to the ED, his travel history of having recently visited West Africa was recorded by a Nurse in the Electronic Health Record (EHR) but due to a system / process / workflow breakdown key members of the care team did not see this vital information. We could go round in circles allaying blame on the EHR, the Nurse or the Physician but this is pointless. Overall it's a system failure and the lesson to learn is how could this have been prevented from the onset and rectified so it doesn't occur again.
I trained in Infectious diseases and saw many different conditions which were rare infectious diseases by all accounts but what was fundamentally at the core in ensuring an accurate differential diagnosis for the symptoms the patients presented with was their travel history. I worked in a tertiary referral hospital for Infectious Diseases where the scenario we were repeatedly faced with was the following: patients came to us having been unwell with their symptoms for several weeks or months and the common diseases had been worked up and ruled out. Yet because no causative agent had been found and the patient was normally worsening they were then referred to our hospital as a last resort as all other options had been exhausted.
What was interesting to see was the way the patients were worked up and examined from the admitting nurse who took a Nursing history (which always included asking about recent travel history) to the Junior Doctors (F1/F2) who took their own history, to the Specialist Registrar and Consultant who would then review the history and often take their own history or ask further questions to the patient and their family in order to gain more information which from their own experience would help assist in making a final diagnosis. Always the recent travel history was investigated and even travel history going back a number of years as well as exposure to other diseases including Infectious diseases and contact with animals or vegetation. You may think all this history taking is overkill but what was interesting on examining the notes of these Physicians and Nurses at different levels of experience was how they differed with essentially the same story being relayed by the patient. A good history and physical examination is fundamental aspect of medicine - unless you ask the correct questions you will not get the answer from the patient. What you are doing is building a puzzle out of clues which will help you find the final piece which you need to complete the puzzle. These difficult or interesting Infectious cases where then taken to a weekly grand round where all the departmental medical and nursing staff would meet to dissect these cases, seek out more information and discuss what the next steps would be for the patient. With so many members of the wider team present for these Grand Rounds from Professors to medical/nursing students with a combination of many hundred years of experience within Infectious Diseases it was fascinating to watch and explore all forms of diseases from around the world and ultimately work out a differential diagnosis and work up for the patient to rule out diseases until the causative disease was identified and the patient successfully treated and discharged
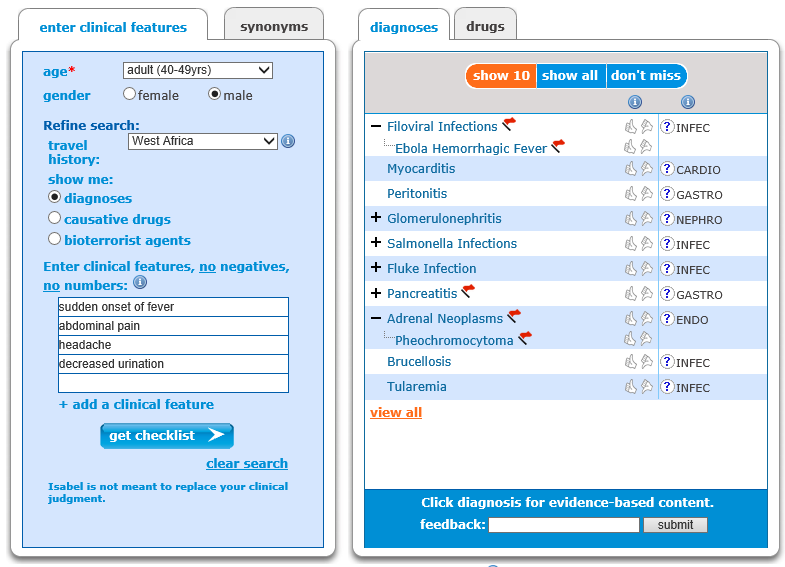
Isabel the diagnosis decision support tool was constructed based on these templates from the Grand Round of working through cases and constructing an accurate clinical picture, creating a differential diagnosis list. Indeed the first data source and detailed part of the database was Infectious Diseases. It was realised in order to make Isabel as powerful as possible that for every disease in the database we needed to attach codes to ensure it was searched accurately by age, gender and region where the Infectious Disease occurred. This also ensured that diseases such as Malaria would only show in regions where malaria is endemic and the same for Ebola. As outbreaks occur and a disease moves to other regions as is endemic in Infectious Diseases the same process can occur with the Isabel database as it is served over the internet we can update the data to ensure its showing real time disease data for symptoms entered and the differential diagnoses list it produces. The Isabel user will initially see we give a search for symptoms based on the region where the Isabel user has set up an account but on the page where the results are generated a new field is made available stating travel history. From the clinical exam and medical history taken the Physician can then alter the region depending on the patients recent travel history and obtain a list of diagnoses from the symptoms entered which are specific to the region the patient has travelled to or from. With Isabel integrated into Electronic Health Records this process can be automatically generated by pulling this information from age, gender, travel history and physical exam fields.
The health care professional is the key in this whole process. From their enquiring minds, asking the appropriate questions, listening to the answers given by the patient, examining the patient and writing detailed documentation of their findings with a good differential list, they ultimately find the best and successful treatment for the patient. Every health professional who then subsequently comes into contact with the patient should be reassessing the history given and the patient’s current symptoms and always have an open mind so as not to prematurely close of all options available to them.
Diagnosis reminder tools such as Isabel are there to assist Physicians in generating a differential diagnosis but what's important and fundamental in preventing diagnosis error is a good physical exam, accurate history taking including recent travel history, tools are only as good as the information which is fed into them and these will help prevent system wide failures.
West Africa travel history for Ebola Dallas Case

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 33 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Isabel DDx Companion with ChatGPT Integration - to help you diagnose even faster
At Isabel Healthcare, we’ve always been driven by one goal: to make clinical reasoning faster,..Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Clinical Decision Support
- Diagnostic Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Clinical Reasoning
- Evidence-based Medicine
- Medical Education
- Patient Engagement
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.





