- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2025
Spotting Stevens-Johnson syndrome - symptoms and causes of SJS and TEN
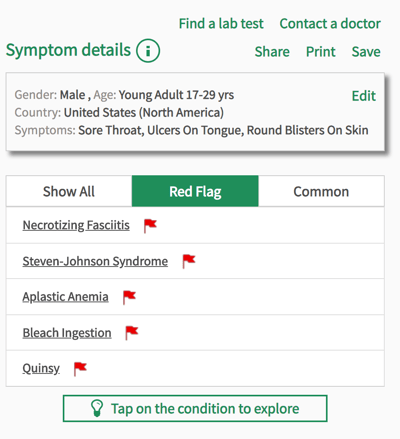
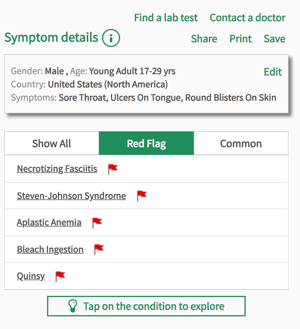 August is the awareness month for Stevens-Johnson syndrome (SJS), an extremely rare and life threatening disease that can develop over mere hours, and is often missed or left untreated for too long. A rare disease is categorized as a disease that affects less than 5 in 10,000 people in the UK, and in the US it is any disease that affects fewer than 200,000 people at any time, which is about 5 in 7,500. SJS affects around 2-6 people in every million, so it certainly passes the rarity test. At Isabel, which started as a charity after the misdiagnosis of a rare disease, we try to shed a light on rare diseases, particularly those that require timely diagnosis, and particularly those that often affect children. In this blogpost we’ll go over the signs and symptoms to spot in SJS, and explain the causes of this serious condition.
August is the awareness month for Stevens-Johnson syndrome (SJS), an extremely rare and life threatening disease that can develop over mere hours, and is often missed or left untreated for too long. A rare disease is categorized as a disease that affects less than 5 in 10,000 people in the UK, and in the US it is any disease that affects fewer than 200,000 people at any time, which is about 5 in 7,500. SJS affects around 2-6 people in every million, so it certainly passes the rarity test. At Isabel, which started as a charity after the misdiagnosis of a rare disease, we try to shed a light on rare diseases, particularly those that require timely diagnosis, and particularly those that often affect children. In this blogpost we’ll go over the signs and symptoms to spot in SJS, and explain the causes of this serious condition.
What is Stevens-Johnson syndrome (SJS)
Stevens-Johnson syndrome, named after the two doctors who first described the disease in 1922, is an autoimmune disorder that manifests as a painful rash on the skin, mucous membranes, and genitals. The disease is often caused by an allergic reaction to certain medications. It can be an over-reaction of the immune system to viral or bacterial infections, and this is more common in children and young adults. Any infection, from the simple flu virus to viral meningitis, can cause an adverse immune response and SJS. Likewise, any drug could at all could cause an allergic reaction, although some are more common than others. The most common drugs to cause SJS are:
- allopurinol
- carbamazepine
- lamotrigine
- nevirapine
SJS is an acute emergency disease, meaning it develops over a matter of hours or days and immediate medical attention should be sought. If left untreated, the skin rash intensifies and blisters, causing painful sores when they burst. The mucous membranes, which run through the digestive tract from the mouth to the anus, also become blistered and ulcerated, making digestion and fluid intake extremely difficult. Eventually, the skin dies and begins to peel off, at which point the body is at a high risk of sepsis and other life threatening complications.
When is it TEN?
SJS is serious enough as it is, but when the reaction is more severe it is then called toxic epidermal necrolysis (TEN). They are the same disease, and are differentiated by the level of damage to the skin. If 1-10% of the skin is damaged, SJS is the diagnosis. Between 10% and 30% is known as an overlap of both SJS/TEN. Anymore than 30% and it is categorized as TEN. The causes and treatment are much the same, which we will go into later on in the blogpost.
Symptoms of SJS
The beginning stages of SJS are somewhat hard to spot as they resemble those of the flu, with a temperature, sore throat and fatigue. Within 1-3 days of this, the mucous membranes in the digestive tract, the genitals and the eye sockets, become inflamed and ulcers or blisters begin to form. This then begins on the skin, where a rash starts forming. The rash is known as a target rash, as small 1 inch round marks form that appear darker in the middle and fade towards the outside, resembling a target. A blister forms from the center and if it pops, causes open sores. The symptoms to look out for are:
- Sore throat
- Fever
- Fatigue
- Stinging eyes
- Ulcers in the mouth or on the lips
- Ulcers or blisters in the genital area
- Small, round, target-like marks and blisters on the skin
- Pain when swallowing
- Vomiting
- Abdominal pain
Diagnosis and treatment of SJS
SJS or TEN is usually diagnosed through a physical examination and history, and on rare occasions a biopsy where some skin is removed to be tested. However, because SJS is an acute condition that must be treated as soon as possible, often the biopsy is not used and diagnosis from examination alone is enough to start treatment. Treatment involves finding the route cause of the reaction, be that an infection or adverse drug reaction. Once the cause is identified, treating the infection and avoiding the medication should stop symptoms from worsening. Managing symptoms then becomes the primary concern. Painkillers, creams and ointments, cold compresses against affected skin, eyedrops, and antiseptic mouthwashes could all be used to help alleviate the pain and irritation of the skin and mucous membranes. Some people are given IV fluids and in some cases food as well, while the body recovers, and to prevent dehydration. Once the reaction stops, the skin begins to recover and regrow within a few days. Full recovery, however, can take weeks or even months, depending on how much skin was damaged. Scarring and pigmentation on the skin is common, and sometimes physiotherapy is needed to regain the movement in the skin.
If you are concerned about any of the symptoms mentioned in this blogpost, particularly if you suspect SJS, place all your symptoms into Isabel and seek medical attention immediately.
Subscribe Here!
Recent Posts
Isabel DDx Companion with ChatGPT Integration - to help you diagnose even faster
At Isabel Healthcare, we’ve always been driven by one goal: to make clinical reasoning faster,..Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Clinical Decision Support
- Diagnostic Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Clinical Reasoning
- Evidence-based Medicine
- Medical Education
- Patient Engagement
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.