- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2025
World Heart Month 2018 | Could I Have Angina?
 February brings with it matters of the heart, in more ways than one. Aside from Valentine’s Day on February 14th, the month also marks a focus on heart health both in the US and the UK. We’ve blogged about Heart Month for the past two years now, on steps you can take to improve your heart health and atrial fibrillation symptoms, and 2018 is no different. This year we’ve chosen another common heart condition which is often ignored or left undiagnosed, as people fear that it may be the sign of a more sinister problem. The truth is, angina is a great warning and a reminder for us to take a look at our overall health and how we’re treating our hearts, so ignoring it can lead to much bigger problems.
February brings with it matters of the heart, in more ways than one. Aside from Valentine’s Day on February 14th, the month also marks a focus on heart health both in the US and the UK. We’ve blogged about Heart Month for the past two years now, on steps you can take to improve your heart health and atrial fibrillation symptoms, and 2018 is no different. This year we’ve chosen another common heart condition which is often ignored or left undiagnosed, as people fear that it may be the sign of a more sinister problem. The truth is, angina is a great warning and a reminder for us to take a look at our overall health and how we’re treating our hearts, so ignoring it can lead to much bigger problems.
What is angina?
Angina is actually a symptom rather than a condition of itself. In the medical field it is known as angina pectoris, and is defined as a chest pain or discomfort that occurs due to coronary heart disease (CHD). We’ve written about CHD in our previous blogposts on heart month, but it is a condition in which the main arteries supplying blood to the heart become partially blocked and hardened by fatty substances called plaques, meaning blood flow to the heart becomes more difficult. This causes angina pains as the blood vessels try to get through the build up of plaques to the heart muscle. CHD and angina are caused by factors such as age, weight, family history and lifestyle. Smoking, high cholesterol, obesity and diabetes all increase your risk of plaque build up and therefore heart disease and angina.
What does angina feel like?
Angina is essentially a warning sign that you are at a higher risk of heart attack or serious heart complications, so it should never be ignored. Angina itself does not cause permanent damage to the heart muscle, but if ignored it can lead to bigger problems. Pain can vary from quite minimal and almost feeling like a bad case of indigestion, to feeling like your heart is stopping and you are suffering a heart attack.
The pain can feel like any of the following:
- a dull ache around your chest
- a sharp pain either side of your heart, or near your ribs
- a tightness in your chest
- feeling like your chest is being squeezed
- a pain spreading from your heart to your neck, jaw, back or even stomach
With the pain or discomfort, you may also experience:
- nausea
- dizziness
- fatigue
- shortness of breath
- wheezing
- sweating
If you haven’t been diagnosed with angina and are experiencing pain in your chest either after exercise or at rest, then you should visit an emergency room as soon as possible. Doctors will be able to assess whether you are having a heart attack, have a serious heart disease, or are suffering from angina.
Types of angina
There are two main types of angina, known as stable and unstable. Stable angina occurs with obvious triggers, such as running, changes in weather or temperature and stress or anxiety. Unstable angina occurs with no obvious triggers, so can happen when you are sitting down and with no warning, for example. If your doctor diagnoses you with stable angina, and you start to have angina attacks with no obvious trigger, you should consult with your doctor again, as you may have developed unstable angina. Some people can have unstable angina from the beginning, but it is more common to develop unstable angina as your angina attacks become more frequent and less obviously defined by triggers as time goes by.
Treatment of angina
Once you have been diagnosed with angina, there are many steps you can take to both alleviate symptoms, and also help prevent the angina getting worse and leading to larger heart issues. Lifestyle changes are the best thing you can do to help your body and your heart, and we’ve blogged about the small changes you can make to your everyday life for heart health before. There are medications as well, however, that will help prevent an attack of angina and relieve the symptoms when an attack occurs.
Nitrates may be prescribed, which relax the arteries and veins around the body and help blood flow to return to a normal rate. Nitrates can be given as regular pills or patches, although continued use of these methods can result in resistance to the medication, so it is recommended to use these in moderation wherever possible. Your doctor will talk through how often you should be taking the nitrate pills or wearing the patches. The most common use of nitrates is in a spray form. When an attack of angina is anticipated or just starting, the nitrate is sprayed underneath the tongue, causing almost instant relaxation of the arteries and therefore easing symptoms.
How do I know if it’s angina or a heart attack?
Simply put, if you haven’t been diagnosed with angina, you simply don’t know, and that is why any symptoms should be taken extremely seriously. Visiting the emergency department means a heart attack can be ruled out, and nitrates can be prescribed, as well as lifestyle recommendations. If you have been diagnosed with angina and have your nitrate spray or medication, you should administer the nitrates as soon as possible after an attack, or even before if a trigger of stable angina is anticipated. If you have taken two doses and the symptoms of an angina attack haven’t eased after a few minutes, then you should call the emergency services immediately.
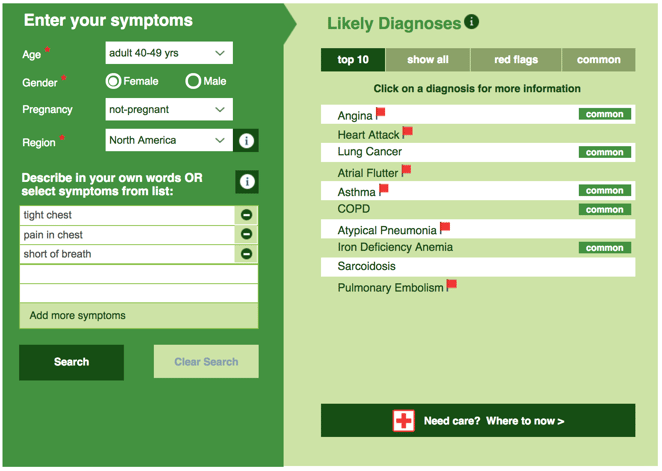
If you are concerned about your heart health at all seek medical attention straight away, as the amount of time you leave before finding help can change the outcome drastically. Placing all your symptoms into the Isabel Symptom Checker to discuss with doctors can help identify the problem. In the meantime, even if you don’t have symptoms, a healthy lifestyle of a diet low in saturated fats and plenty of exercise, among other things, can help prevent symptoms like angina developing in the first place.

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 33 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Isabel DDx Companion with ChatGPT Integration - to help you diagnose even faster
At Isabel Healthcare, we’ve always been driven by one goal: to make clinical reasoning faster,..Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Clinical Decision Support
- Diagnostic Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Clinical Reasoning
- Evidence-based Medicine
- Medical Education
- Patient Engagement
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.