- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2025
Differential Diagnosis Aplastic Anemia - 1 Minute Read
 Aplastic anemia is a rare life-threatening disorder with hypocellular bone marrow, where the bone marrow cannot make enough new blood cells. This hypocellular bone marrow results in pancytopenia, which is low reticulocyte, granulocyte and platelet counts. We’ve written about pancytopenia before if you’d like to know more about that. Each year between 2-5 people per 1 million are affected by aplastic anemia. Aplastic anemia occurs most frequently in young adults between 10-25 years old, as well as patients older than 60 years.
Aplastic anemia is a rare life-threatening disorder with hypocellular bone marrow, where the bone marrow cannot make enough new blood cells. This hypocellular bone marrow results in pancytopenia, which is low reticulocyte, granulocyte and platelet counts. We’ve written about pancytopenia before if you’d like to know more about that. Each year between 2-5 people per 1 million are affected by aplastic anemia. Aplastic anemia occurs most frequently in young adults between 10-25 years old, as well as patients older than 60 years.
Causes of aplastic anemia
In 70-80% of cases the disease is acquired and unable to be related to identifiable causes or is caused by idiopathic reasons. Inherited aplastic anemia accounts for the other 15-20% of cases.
All bone marrow contains hematopoietic stem cells that divide, differentiate and become red blood cells, white blood cells, or platelets. Researchers think there is an autoimmune element where an initiating event triggers immune-mediated destruction of the hematopoietic stem cells by the T-lymphocytes. They target these primitive stem cells and prevent them developing into mature blood cells, and the bone marrow becomes replaced by fat. The affected person develops pancytopenia.
Signs and symptoms of aplastic anemia
Aplastic anemia can be insidious, developing over weeks to months, or acute. The symptoms the patient presents with include:
- anemia, manifesting as fatigue, pallor, weakness, dyspnea, and exercise intolerance
- thrombocytopenia, which can cause symptoms of easy bruising, skin or mucosal haemorrhage, petechiae, epistaxis, and menorrhagia
- fever or infection caused by neutropenia
Symptoms can be very similar to many other diseases so using the Isabel DDx Generator can help you formulate an accurate differential diagnosis to ensure you consider all possible diseases and make a correct diagnosis.
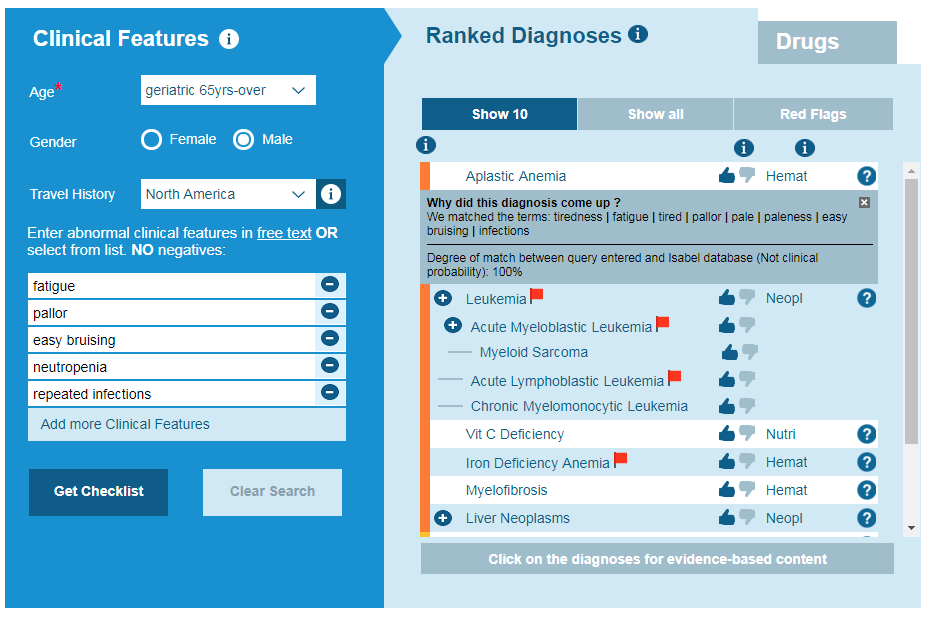
Isabel DDx Generator – aplastic anemia
Taking a history and physical examination
It is important to ask about any medications and recreational drug use, past medical and family history. Examine the patient for short stature and congenital anomalies. To make the diagnosis you need to distinguish between inherited and acquired aplastic anemia. The patient must have pancytopenia with involvement of 2 or more lineages in peripheral blood cells, and a hypocellular bone marrow without dysplasia or fibrosis. If the patient has idiopathic aplastic anemia then you need to exclude other causes of pancytopenia with hypocellular bone marrow and inherited bone marrow failure syndromes. A diagnosis can be confirmed through taking a bone marrow biopsy.
Differential diagnosis
Symptoms of aplastic anemia are common with other disorders and so reviewing your differential diagnosis for these conditions, and ruling out other disorders in order to make an accurate diagnosis is important.
Myelodysplastic syndromes
These are a rare group of blood disorders which result from the improper development of blood cells within the bone marrow. They enter the circulatory system and due to their improper development, the individuals affected have abnormally low blood counts. It can be difficult to distinguish between myelodysplastic syndromes and aplastic anemia.
Paroxysmal nocturnal hemoglobinuria (PNH)
This is caused by the hemolysis of red blood cells, which in turn causes repeated episodes of hemoglobinuria. Hemoglobin is the red iron-rich pigment in haemoglobin and as a result the patient will have dark-colored or bloody urine. This finding is most often seen in the morning as the urine is more concentrated when the patient has been asleep overnight. Patients with PNH can also develop life-threatening blood clots.
Genetic disorders
Aplastic anemia may occur as part of an inherited disorder. Some key genetic disorders to be aware of and investigate if a child or adult presents with aplastic anemia include Fanconi anemia, Schwachman-Diamond syndrome and ataxia-pancytopenia syndrome. Fanconi anemia includes pancytopenia, cardiac and renal abnormalities and skin pigmentation changes.
Treatment of aplastic anemia
Depending on the severity of aplastic anemia the treatment options are wide and may consist of supportive care only, immunosuppressive therapy or hematopoietic cell transplantation. Aplastic anemia patients may require inpatient care during periods of infection. One third of patients with aplastic anemia do not respond to immunosuppressive therapy. Pregnant women with aplastic anemia have a 33% risk of relapse. Those patients who have aplastic anemia require regular follow-up appointments to monitor blood counts and drug side effects. They will also require blood transfusions to maintain their blood counts.
Complications
Aplastic anemia has a high mortality rate if not treated. Death can result from infection and haemorrhage. Prompt recognition and diagnosis of aplastic anemia is key to ensuring the patient receives the treatment they need, and to prevent them from progressing to further complications that can result if the condition isn’t diagnosed.

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 33 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Isabel DDx Companion with ChatGPT Integration - to help you diagnose even faster
At Isabel Healthcare, we’ve always been driven by one goal: to make clinical reasoning faster,..Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Clinical Decision Support
- Diagnostic Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Clinical Reasoning
- Evidence-based Medicine
- Medical Education
- Patient Engagement
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.



