- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2020
Malaria | 1 Minute Read | Causes, symptoms and treatment
 Malaria is a parasitic infection caused by protozoa of the genus Plasmodium. There are five species which can infect humans, but Plasmodium falciparum is the most life-threatening. It is transmitted to humans through the bite of an infected female Anopheles mosquito, but could also potentially be transmitted by blood transfusion or organ transplants.
Malaria is a parasitic infection caused by protozoa of the genus Plasmodium. There are five species which can infect humans, but Plasmodium falciparum is the most life-threatening. It is transmitted to humans through the bite of an infected female Anopheles mosquito, but could also potentially be transmitted by blood transfusion or organ transplants.
Background
Malaria is a major course of death in tropical and sub-tropical countries. In 2012, there were an estimated 207 million malaria cases which resulted in 627,000 deaths, of which 80% occur in African children. To reduce the numbers of malaria cases worldwide, it is essential to have prompt and effective diagnostic methods including the history of a patient, as well as clinicians who recognise the symptoms so that Malaria can be promptly investigated and ruled out of a differential diagnosis. Since 2000, there has been a lot of international investment into controlling and ultimately eliminating malaria. This has seen mortality rates fall by 42% in all age groups, with an estimated 90% of deaths averted in children under 5 years of age in sub-Saharan Africa.
World Map showing Malaria distribution and areas where it is being controlled or eliminated
Malaria etiology and causes
There are five Plasmodium species which cause human malarial disease, and they can be found in different parts of the world:
- P falciparum – widespread on the tropic region of sub-Saharan Africa, some areas in Southeast Asia, Oceania and the Amazon basin in South America.
- P vivax – predominantly found in Asia, the Americas, some parts of Eastern Europe and North Africa
- P ovale - found in tropical western and Central Africa and islands in the West Pacific
- P malariae – similar to P falciparum but has a lower prevalence worldwide
- P knowlesi – found in parts of southeast Asia
Malarial parasites enter the body via a mosquito bite and proceed to digest the red blood cell (RBC) proteins, altering the red blood cell membrane. This causes hemolysis, increased splenic clearance and anemia. The lysis of the red blood cell also stimulates and releases cytokines and tumor necrosis factor-a.
Symptoms of Malaria
- fever or a history of fever. A cycle can develop, consisting of chills and rigors followed by fever and sweats with associated tachycardia.
- headaches
- weakness
- myalgia
- arthralgia
- anorexia
- diarrhea
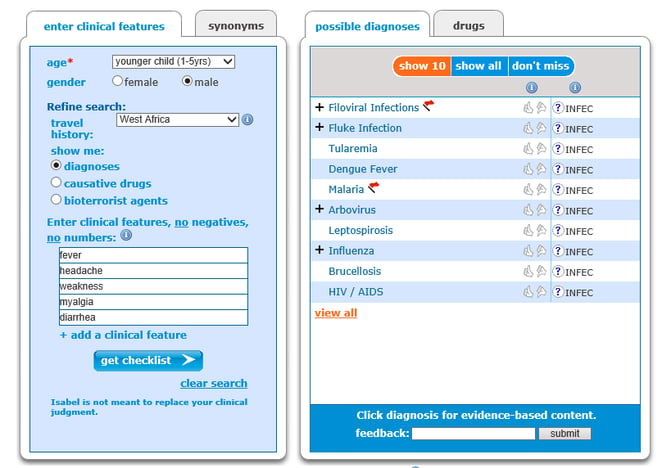
Isabel differential diagnosis showing why Malaria should be considered for key symptoms or from patients returning from endemic regions
Malaria should be considered in any patient who lives in malaria endemic regions or from travellers who have recently returned from holiday to these areas. As you can see, the symptoms of Malaria are extremely common symptoms for a large range of conditions, which is why travel history and geographical information is so important to establish.
How should I test for Malaria?
Tests to order when diagnosing Malaria include:
- Peripheral smear - thick and thin stained blood smear findings
- Rapid antigen diagnostic testing
- Complete blood count – may show thrombocytopenia, anemia and leucocytosis
- Liver function tests – may show elevated transaminases, elevated bilirubin and elevated lactate dehydrogenase
- Blood chemistry – hyponatremia, increased creatinine and hypoglycemia
How is Malaria treated?
If diagnostic confirmation via laboratory testing is not possible then treatment can be based on clinical suspicion. Treatment is sometimes initiated before laboratory testing is confirmed as the earlier treatment is given, the quicker the resolution of the illness and the easier it is to prevent the disease course worsening. For up to date treatment guidelines it is best to consult with a pharmacist and the laboratory who have tested the peripheral blood smears, as treatment does depend on the parasite type found on the smear.
Fever can be treated with antipyretics to alleviate some discomfort for the patient whilst the antimalarial medication starts to take effect. If patients are unable to tolerate fluids orally then carefully controlled intravenous fluids should be prescribed with glucose added to prevent hypoglycemia which may occur with malaria.
Since 2013, exchange transfusion as an adjunct to treating antimalarials for severe cases of malaria with respiratory, renal or cerebral compromise is no longer recommended. A review of the studies available showed no difference in the means of survival between those who received an exchange transfusion as well as antimalarials, compared to those who didn’t receive an exchange transfusion.
Complications of Malaria
If the degree of parasitemia is severe or the malaria progresses due to not being diagnosed quickly enough, then other complications can occur, including:
- Cerebral malaria – altered level of consciousness, focal neurological findings and seizures
- Renal failure
- Blackwater fever – severe clinical syndrome including intravascular hemolysis, hemoglobinuria, acute renal failure
- Anemia
- Respiratory distress
- Bacterial infection
Prevention is better than cure
Avoidance of contact with mosquitoes is the prime factor for prevention, and should be encouraged for any patient living in or visiting countries at risk of Malaria.
- Avoid exposure at times when mosquitoes are at their most active like dusk and dawn
- Avoid scented cosmetics and perfumes
- Wear long sleeve tops, trousers and hats
- Use insect repellents
- Avoid camping near water such as ponds and swamps
- To prevent mosquitoes getting into the house if doors are left open, use netting or beads over the door.
- Travelers to malaria endemic regions should use malaria prophylaxis which varies according to the region and/or countries the traveler is visiting.
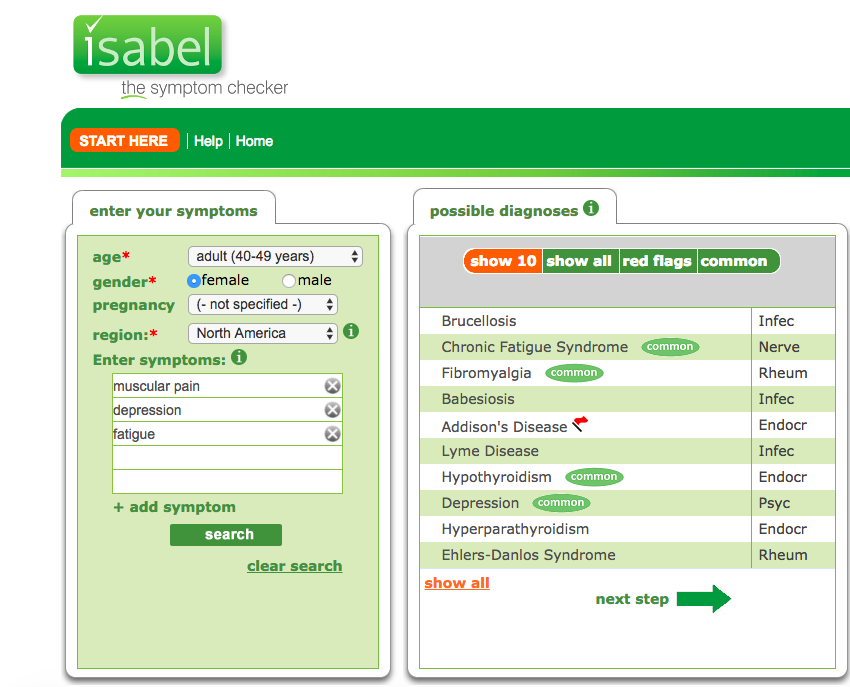
Have you read our eBook with tips on implementing a diagnosis decision support system like Isabel into your institution?
Top Image Attribution:
"Aedes aegypti mosquito" (CC BY-NC-ND 2.0) by Sanofi Pasteur

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 28 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..Webinar: Using Virtual Triage To Transform Patient Access
Outdated contact centers are posing problems for today's health systems. As longer hold times..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Diagnostic Decision Support
- Clinical Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Medical Education
- Patient Engagement
- Clinical Reasoning
- Evidence-based Medicine
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.