- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2020
1 Minute Read - Mitochondrial Disease - Need for Timely Diagnosis
 Results of a recent survey published in the journal Neurology Genetics, on patients with mitochondrial disease, have stated that genetics identify the ‘diagnostic odyssey’ experienced. Diagnostic odyssey is defined as the time taken between a patient first developing symptoms and receiving a correct medical diagnosis. 210 patients participated in the survey, all of whom had physician diagnoses of mitochondrial disease and were recruited through the Rare Diseases Clinical Research Network. The results were alarming:
Results of a recent survey published in the journal Neurology Genetics, on patients with mitochondrial disease, have stated that genetics identify the ‘diagnostic odyssey’ experienced. Diagnostic odyssey is defined as the time taken between a patient first developing symptoms and receiving a correct medical diagnosis. 210 patients participated in the survey, all of whom had physician diagnoses of mitochondrial disease and were recruited through the Rare Diseases Clinical Research Network. The results were alarming:
- On average patients saw 8 clinicians before receiving a diagnosis
- Over half of the participants (55%) reported a misdiagnosis during their journey to a correct diagnosis
- The most common misdiagnoses were: psychiatric disorder (13%), fibromyalgia (12%), chronic fatigue syndrome (9%), and multiple sclerosis (8%)
- More than 800 individual symptoms were reported by the respondents. The most common symptoms which prompted the respondent to seek medical attention were: muscle weakness (62%), fatigue (56%), walking difficulty (39%), droopy eyelids (33%), and impaired coordination (32%)
- To reach a correct diagnosis, participants underwent a variety of tests. including blood tests (84.8%), muscle biopsy (71%), MRI (60.5%), and urine organic acid collection (38.6%). In addition, some also had mitochondrial DNA sequencing performed (39.5%) sequencing of nuclear gene(s) (19%), or whole-exome sequencing (11.4%)
- The most frequent diagnoses were myopathy (22%), chronic progressive external ophthalmoplegia (10%), and mitochondrial encephalopathy, lactic acidosis and stroke-like episodes (MELAS) (9%).
What are mitochondrial diseases?
Mitochondria are the energy power houses of the cells within the body. Each cell has several thousand mitochondria which process oxygen and convert substances from the foods we eat into energy. Mitochondria produce 90% of the energy the body needs to function. Mitochondrial diseases are chronic, genetic and often inherited disorders which occur when the mitochondria fail to produce enough energy for the body to function properly. As each cell has its own mitochondria, the spectrum of diseases caused by these disorders is wide. Cells from nerves, muscles, kidney, liver, brain, eyes and ears can be affected and mitochondrial diseases include autism and Parkinson’s disease.
A brief history of mitochondrial diseases
The first mutation in mitochondrial DNA was only identified in 1988, so research is still very much ongoing in the field as we develop our understanding of these complex diseases. A lot of the earlier thinking was that mitochondrial diseases were always present from birth, as the sickest infants often died in infancy when diagnosed. Over recent years, however, we are seeing that mitochondrial diseases can appear at any age, depending on a range of factors and the specific type of mitochondrial disease. What’s more, these diseases are not as rare as we first imagined, but the disease is not diagnosed as it isn’t considered in the patient’s differential diagnosis workup. With advances in genetics and molecular biology in the past decade more has been understood about the complexity of mitochondrial diseases and how widespread their symptoms and manifestations can be, but there remains a lack of physician and public awareness.
How common are mitochondrial diseases?
One in 5,000 individuals has a mitochondrial disease, and around 1,000 to 4,000 children are born in the United States with one. In the United Kingdom, there are around 150 births per year where the mother is at risk of transmitting mitochondrial disease to her child, and in the US that figure is 800. These figures are more than likely conservative estimates, as there are so many variations and subsets of mitochondrial diseases and some are extremely rare; the very rare subsets may not be detected before the patient dies, as some kinds of mitochondrial disease can cause death at an early stage.
What are the symptoms of mitochondrial diseases?
Symptoms vary greatly, depending on which cells of the body are affected by the mitochondrial disease. Patient’s symptoms can be mild or severe, can involve one or more organs and can occur in all ages. Even patients from the same family who have the same mitochondrial disease can have different symptoms, onset and severity of their symptoms. Generally, symptoms can include:
- poor growth
- muscle weakness
- fatigue
- muscle pain
- exercise intolerance
- seizures
- gastrointestinal manifestations such as diarrhea, constipation, or vomiting
- autism
- vision problems
- lactic acidosis
- developmental delay or dementia
- increased risk of infection
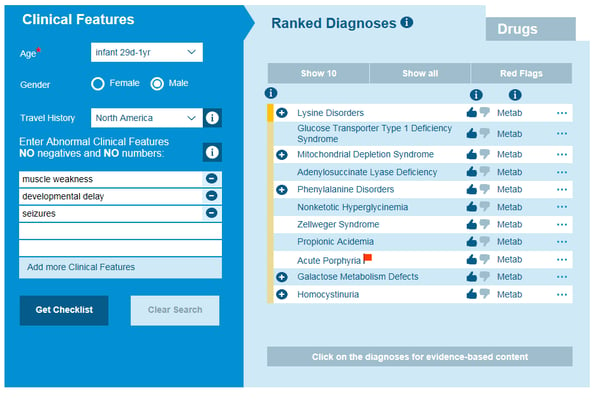
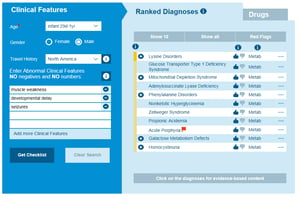
Causes of metabolic diseases in an Infant with developmental delay, myopathy and seizures
How are mitochondrial diseases diagnosed?
As was supported with the survey, making a diagnosis early and referring to a specialist is very important. Mitochondrial diseases affect many organs and tissues of the body and there is no single laboratory or diagnostic test that confirms a mitochondrial disease. In the survey, 56.7% of the respondents first consulted a primary care physician with their symptoms compared to 35.2% who first went to a specialist. This shows the need for primary care physicians to be aware of mitochondrial diseases and how widely their symptoms can present and mimic other disorders. Common and rare diseases should be considered on their differential diagnosis to ensure an appropriate specialist is referred to for the patient’s presenting symptoms. At the time of diagnosis, the survey showed that 55.2% of participants received their diagnosis from a neurologist, 18.2% from a clinical geneticist, and 11.8% from a metabolic disease specialist.
The initial steps to ensuring an accurate and timely diagnosis for a mitochondrial disease are:
- complete review of family history
- complete physical examination
- neurological examination
- metabolic examination including blood and urine tests
Depending on presenting symptoms and which organs and tissues are affected then appropriate secondary testing may include:
- MRI for neurological symptoms
- Retinal exam for vision
- EKG or Echo for heart disease
- Genetic DNA blood testing
- Skin or muscle biopsies
Treatment of mitochondrial diseases
Mitochondrial diseases cannot yet be cured. Treatment is aimed at reducing symptoms and slowing the decline in effects on health. Each mitochondrial disease has its own management and often the management must be tailored to the individual, as what works for one person with that disease may not work for another. Sometimes the mitochondrial disease flare-up can be activated by triggers including cold exposure, lack of sleep, excessive exercise, alcohol use, or stress. Learning what triggers an episode is useful in ensuring the trigger is avoided.
Outcomes
Some people have normal lives and life expectancy with minimal flare-ups and overall effect on everyday life, whilst others can have drastic changes in their health, having a profound impact on their lives. Mitochondrial diseases are complex and can present in a variety of different ways. The survey shows that the process of obtaining a mitochondrial disease diagnosis can take many years and involve multiple doctor referrals. Diagnostic delay can be overcome by ensuring that a differential diagnosis generator like Isabel is consulted when generating the differential diagnosis, to ensure rare and common causes of disease are considered for the symptoms with which the patient presents. Many of these respondents had invasive and painful tests performed to obtain a diagnosis. By working through a differential diagnosis and evaluating the patient’s symptoms for potential diagnoses, the tests needed to confirm a diagnosis can be narrowed down. The exploration of a patient’s symptoms, history, and physical examination is imperative to making a diagnosis in a timely manner, as many metabolic diseases have unique features that enable a diagnosis to be made if a proper workup and history is obtained.

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 28 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..Webinar: Using Virtual Triage To Transform Patient Access
Outdated contact centers are posing problems for today's health systems. As longer hold times..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Diagnostic Decision Support
- Clinical Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Medical Education
- Patient Engagement
- Clinical Reasoning
- Evidence-based Medicine
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.