- Privacy Policy
- Terms & Conditions
- Contact us
- ©Isabel Healthcare 2020
1 Minute Read | Late Pregnancy Bleeding | Differential Diagnosis
Late pregnancy bleeding, or antepartum hemorrhage is vaginal bleeding which occurs after 20 weeks of gestation and is reported in 2-5% of all pregnancies. Vaginal bleeding occurring at this point in later pregnancy is associated with increased maternal risks, including maternal morbidity secondary to acute haemorrhage, or operative delivery. Increased fetal risks can occur due to uteroplacental insufficiency or preterm birth. Successful management depends on accurate identification of the cause of the bleeding and timely intervention according to severity of the condition.
Assessment of Late Pregnancy Bleeding
The clinical presentation of the vaginal bleeding will vary depending on the cause. Any bleeding in pregnancy is a cause for concern and should be thoroughly investigated. The assessment of the vaginal bleeding aims to distinguish minor causes from those which are more serious. Bleeding may present:
- as minor spotting
- as blood stained amniotic fluid
- as blood flow similar to menstruation
- as hemodynamic instability due to massive haemorrhage
- with sudden onset, but may be non-acute
- after sexual intercourse or if the patient suffers a trauma such as a fall, vehicle accident or violence.
In addition to the bleeding, other symptoms may occur, including:
- abdominal pain
- back pain
- abdominal cramping
- uterine contractions
- decreased fetal movement
- dilatation of the cervix.
Ensure an accurate past medical history is obtained asking about factors associated with late pregnancy loss including diabetes, epilepsy, cyanogenic heart disease, thromboembolic diseases, other episodes of preterm labor or premature rupture of membranes or cholestasis in pregnancy. Check whether the patient is using any over the counter or prescription medications. Carry out a full physical examination of the abdomen and pelvis. Avoid any digital exam until placenta previa has been ruled out via ultrasound.
Differential Diagnosis
The following tests and evaulations should be carried out which will allow you to generate a differential diagnosis, and make a final diagnosis which can be treated in a timely manner preventing further complications to mother and fetus:
- Visual estimate of blood loss
- Ultrasound to determine location of placenta and identify bleeding source
- Continuous fetal monitoring
- Laboratory tests including haematocrit, platelet count, fibrinogen level, coagulation, blood type and antibody screening.
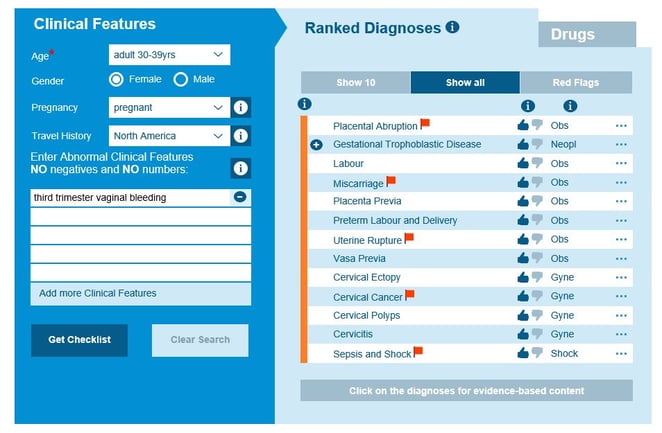
This thorough history and physical examination, including observations and tests, will help you differentiate minor cases from those which are more serious causes of vaginal bleeding. You can now form and consider your differential diagnosis. Placing the clinical features into Isabel will help you with your differential diagnosis and help make sure no possible diagnoses are missed.
Normal labor
Cervical dilatation is seen with a small amount of blood or blood-tinged mucus known commonly as ‘the bloody show.’
Spotting/minor bleeding
commonly seen in pregnant women after sexual intercourse or if a digital vaginal examination has been carried out.
Placenta previa
This presents with sudden painless vaginal bleeding, often after sexual intercourse. Initial bleed is unlikely to cause hemodynamic instability or fetal harm, but the bleeding can range from minor to massive haemorrhage. Bleeding is normally intermittent rather than continuous. Number of bleeding episodes has no correlation to the degree of placenta previa. The incidence of placenta previa increases with age, parity, tobacco use and previous number of caesarean deliveries. Placenta previa should be suspected in all women with vaginal bleeding after 20 weeks gestation, and those who have a low-lying placenta on second trimester ultrasound. Diagnosis is confirmed by transvaginal ultrasound.
Placental abruption
Symptoms vary, and the patient may be asymptomatic. Common presentation is mild, nonacute bleeding in second or third trimester. Vaginal bleeding may or may not be present. Bleeding varies from small amount to massive haemorrhage. Other symptoms may include abdominal pain, uterine tenderness, or hyper tonic uterus. Placental abruption may present as preterm labor. Blood stained amniotic fluid or membrane rupture may present in some cases. Associated risk factors for placental abruption include use of tobacco or cocaine, chronic hypertension, preeclampsia, thrombophilia, abdominal trauma and previous abruption in an earlier pregnancy.
Vasa previa
Presents as painless vaginal bleeding during amniotomy or spontaneous rupture of the membranes. Hemorrhage is fetal blood and loss can occur rapidly.
Uterine rupture
This can sometimes occur in normal active labor but can also be seen in later pregnancy. Symptoms may be subtle and include abdominal pain and vaginal bleeding which are difficult to distinguish from normal labor. A leading indicator of uterine rupture is a deterioration of the fetal heart rate and a loss of fetal station on vaginal exam. Intra-abdominal bleeding can lead to hypovolemic shock and death.
Preterm labor
Regular uterine contractions between 20 and 37 weeks gestation indicate preterm labor. Patients may have painful contractions if they are sustained. Make the diagnosis of preterm labor based on regular uterine contractions with descent of presenting fetal part, progressive dilation and cervical effacement and gestational age below 37 weeks.
Pregnancy loss
Miscarriage or pregnancy loss may present with vaginal bleeding or history of vaginal bleeding. Patients may also have pelvic pain and abdominal pain. Findings on transvaginal ultrasound may include funnelled cervix, visible products of conception in the cervix or vagina and absent fetal cardiac activity. The pregnant woman may be asymptomatic or experience vaginal bleeding, decreased fetal movement, decreased symptoms of pregnancy, cramping and labor.
Other related disorders which have possible underlying symptoms of vaginal bleeding in late pregnancy include cervicitis, cervical ectropion, cervical polyps and cervical cancer.
Treatment and Outcomes
Once the diagnosis has been made then the treatment plan will vary dependent on the final diagnosis. With conditions of vasa previa and uterine rupture urgent surgery will be required to deliver the baby by caesarean. With placental abruption, depending on the gestation of the patient, a decision will be made either to deliver the baby urgently or if the abruption is mild then to monitor the patient closely in hospital especially if the patient is under 34 weeks gestation.
As the differential diagnosis for late pregnancy vaginal bleeding can be so wide in terms of severity of potential diagnoses, it is important to assess the patient thoroughly and carry out investigations in a timely manner, to prevent any complications occurring to the mother and child. The don’t miss diagnoses which are red flagged on Isabel’s differential diagnosis serve as a reminder of which diagnoses to investigate as a matter of urgency when a pregnant woman presents with late pregnancy vaginal bleeding.

Mandy Tomlinson
Mandy has worked for Isabel Healthcare since 2000. Prior to this, she was a Senior Staff Nurse on the Pediatric Infectious disease ward and high dependency unit at one of London's top hospitals, St Mary’s in Paddington which is part of Imperial College Healthcare NHS Trust. Her experience in the healthcare industry for the past 28 years in both the UK and USA means she's a vital resource for our organization. Mandy currently lives and works in Scottsdale, Arizona.
Subscribe Here!
Recent Posts
Virtual Triage: Do more questions lead to better patient outcomes?
One of the common misconceptions related to virtual triage / symptom checker tools is that the more..Webinar: Using Virtual Triage To Transform Patient Access
Outdated contact centers are posing problems for today's health systems. As longer hold times..List Of Categories
- Differential Diagnosis Decision Support
- Differential diagnosis
- Symptom Checker
- Symptoms
- Medical Error
- Patient Disease Information
- Disease
- Diagnostic Decision Support
- Clinical Decision Support
- Isabel 1 Minute Read
- Diagnosis Error
- Diagnosis Skills Cases
- Healthcare Informatics
- Medical Education
- Patient Engagement
- Clinical Reasoning
- Evidence-based Medicine
- Symptom Triage
- Nurse Practitioner Education
- Nursing Decision Support
- Partnership
- Public Health
- COVID-19
- EHR
- Patient Empowerment
- Patient Safety
- rare disease

Start your FREE Trial today
Try the Isabel Pro DDx generator for 30-days - no payment card details required.




